Our Mission
Our mission at the lab is to revolutionize the treatment of heart diseases through the development of cutting-edge tissue engineering materials and devices. We strive to push the boundaries of current medical technology by creating new and innovative solutions that will improve the clinical outcomes of those suffered from advanced heart failure. Our goal is to design and develop materials and devices that will not only repair damaged tissue, but also promote long-term healing and regeneration. We are dedicated to advancing the field of tissue engineering and making a positive impact on the health and well-being of patients around the world.
Tissue Engineering
The paramount objective of our research endeavors is to create a tissue-engineered heart as a therapeutic intervention for patients suffering from end-stage heart failure. By replacing the diseased heart with a tissue-engineered construct, we aim to restore cardiac function and improve the quality of life for these individuals. As a crucial step towards this ultimate goal, we are currently focusing on the development of a tissue-engineered cardiac patch, which aims to promote in-situ myocardial regeneration and functional restoration. Through the use of state-of-the-art techniques and cutting-edge materials, our team is committed to pushing the boundaries of current medical technology and advancing the field of tissue engineering to benefit patients worldwide.
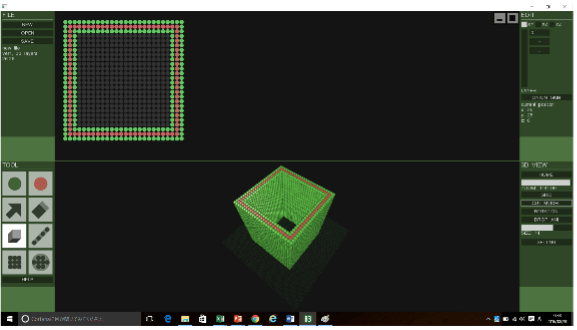
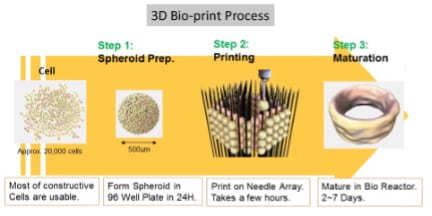
1.) 3D Bioprinter Technology
Novel three-dimensional (3D) bio-printers, such as Regenova/S-Pike (Cyfuse), have been developed and have become available for use. The 3D bio-printer is a robotic system that enables the creation of 3D cellular structures by precisely placing cellular spheroids in fine needle arrays, known as the “Kenzan method,” according to pre-designed 3D data. This system allows for the production of any shape of 3D cellular structure with any desired cell lines in any desired coordinates, as long as they fall within the needle array field. As one of our projects, we have develop a three-layered cardiac patch that possesses a configuration similar to native myocardial tissue and has the potential to promote in-situ, site-specific myocardial regeneration and expedite functional restoration. Unlike other homogenous solid organs, such as the liver or kidney, the human heart has a highly complex configuration with a variety of sophisticated physiological functions, including but not limited to the conduction system, myocardium, and valvular structures, which pose significant limitations in the field of tissue engineering and cardiac surgery. However, the 3D bio-printing system has the potential to overcome these limitations and be a breakthrough in this field.
2.) Cardiac magnetic resonance imaging (CMR)
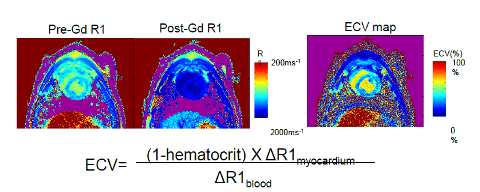
One of our key collaborators, Dr. Keigo Kawaji at Illinois Institute of Technology, is an expert for CMR and a scientist to develop, validate, and evaluate new CMR technologies. Our group established a novel CMR protocol to assess regional cardiac physio-mechanical properties. Strain-encoding (SENC), rest perfusion and T1 Mapping by modified Look-Locker inversion (MOLLI) recovery for extracellular volume fraction (ECV) calculation were effective in assessing the regional and biological myocardial function of a remodeled tissue engineered scaffold. SENC allows rapid and accurate quantification of regional myocardial function. Quantitative CMR perfusion imaging is a powerful tool in the assessment of regional myocardial blood flow. Lastly, the T1-mapping using MOLLI is an emerging technique is a highly sensitive method to quantify the extent of fibrosis, and it will enable us to detect the delicate remodeling process of patch. We apply these techniques to assess blood perfusion, contractility of the patches and extent of fibrosis in the implanted tissue engineered patch.
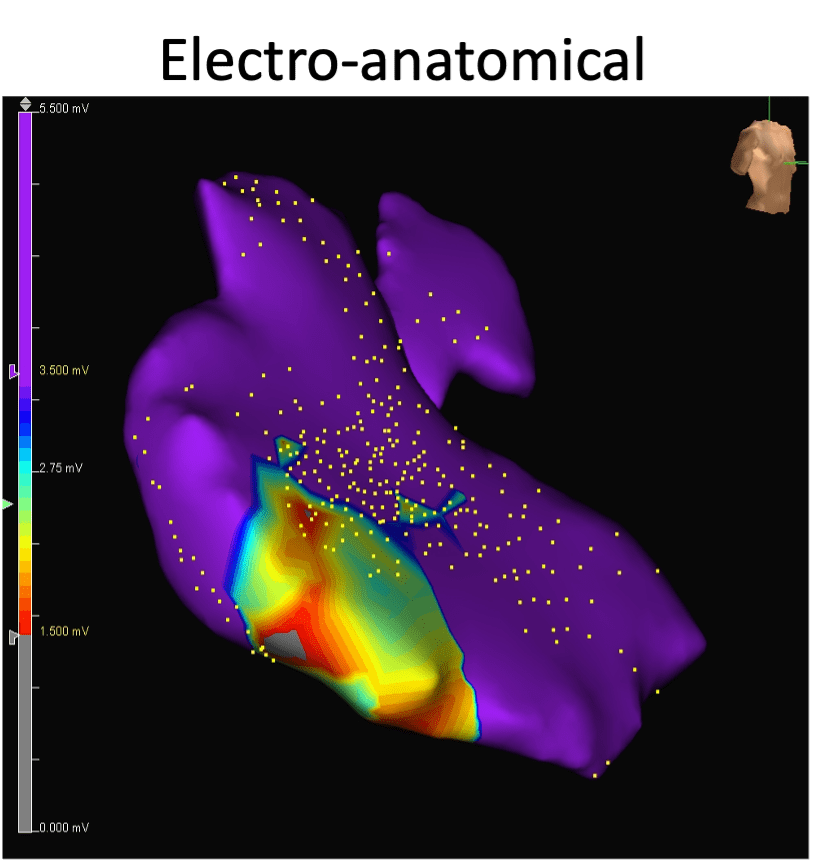
3.) Electromechanical Mapping
Our group have established electromechanical mapping assessment methods in a porcine preparation to evaluate electrical activity as well as regional contractility of implanted patches. Electromechanical mapping was performed using a commercial system; the Velocity Ensite mapping system (St Jude Medical, Inc, St Paul, Minn).The system utilizes synchronous extracorporeal magnetic fields projected into the thoracic space to determine the location and orientation of a sensor mounted near the distal electrode of a deflectable bipolar mapping catheter which can be used to access the endocardial or epicardial surface. This technique allows to detect the implanted tissue engineered patch area accurately and assess meticulous electromechanical activity. In our previous study, a decellularized cardiac patch incorporated with a hydrogel containing a growth factor was tested in the porcine model and the implanted patch was assessed with the electromechanical mapping system. The patch area demonstrated both contiguous and heterogeneous voltage with the adjacent non-patch myocardium. We apply these techniques to assess regional mechanical mapping and contractility in the implanted tissue engineered patch.
Clinical Research Studies
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
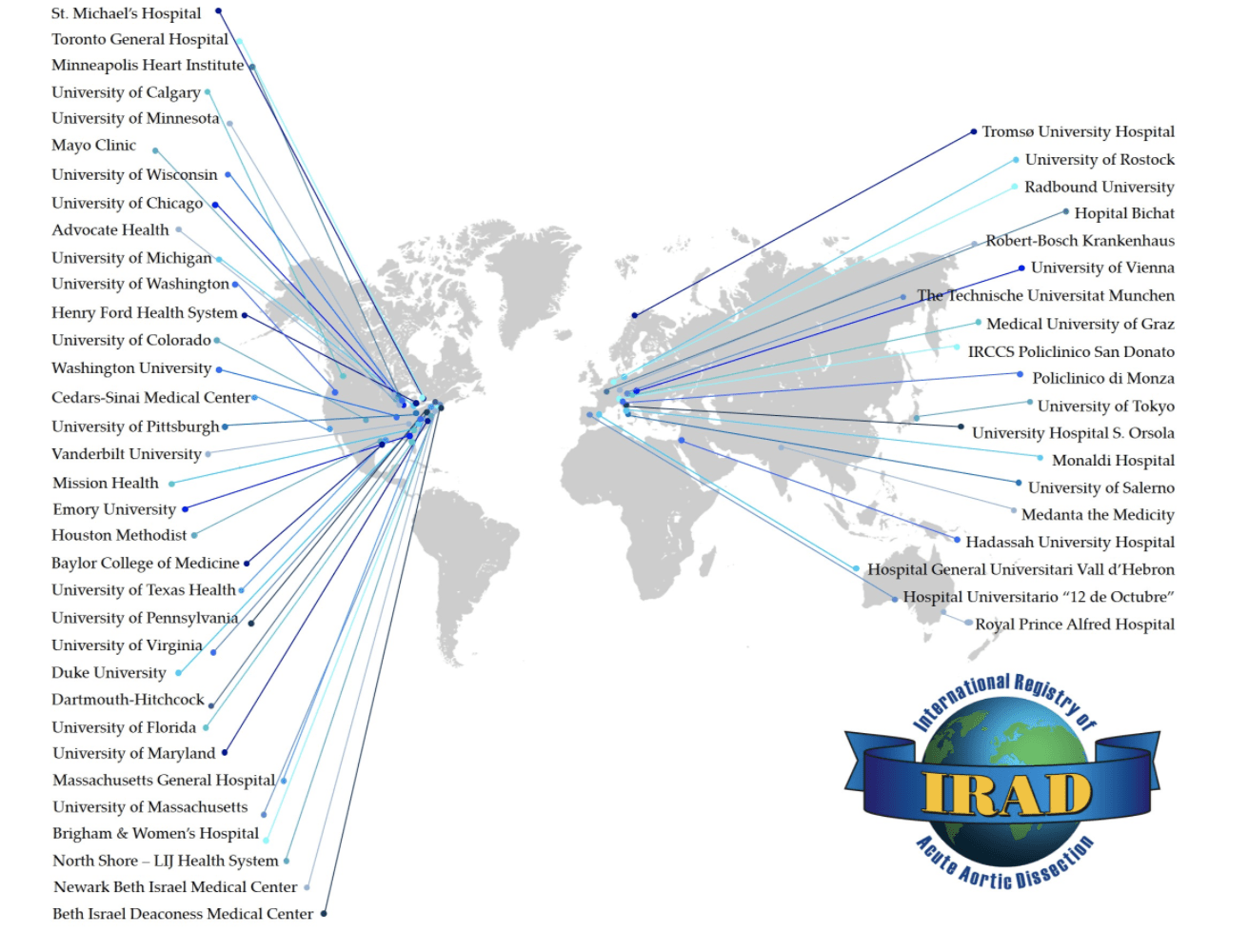
The International Registry of Aaortic Dissection (IRAD)
The International Registry of Acute Aortic Dissections (IRAD) is a consortium of research centers that are evaluating the current management and outcomes of acute aortic dissection. It was established in 1996, and currently has over 30 large referral centers in 11 countries participating in the registry. The main purpose of IRAD is to assess the etiological factors, modes of presentation, clinical features, treatment, and hospital outcomes of patients with acute aortic dissection around the world.
Dr. Ota is the principle investigator for the study at the University of Chicago Medical Center. IRAD investigators have collectively published over 55 articles in peer-reviewed journals.
NuPulse
The International Registry of Acute Aortic Dissections (IRAD) is a consortium of research centers that are evaluating the current management and outcomes of acute aortic dissection. It was established in 1996, and currently has over 30 large referral centers in 11 countries participating in the registry. The main purpose of IRAD is to assess the etiological factors, modes of presentation, clinical features, treatment, and hospital outcomes of patients with acute aortic dissection around the world.
Dr. Ota is the principle investigator for the study at the University of Chicago Medical Center. IRAD investigators have collectively published over 55 articles in peer-reviewed journals.